The endocrine system has glands that secrete hormones. Hormones are chemical messengers that enter the blood and carry messages that act upon the cells and cause the secretion of the cells (1).
Hormones carry proteins and receptor signals to other cells (1).
One type of endocrine gland is the exocrine gland. The exocrine glands secrete products into a duct. These secretions exit the body either as sweat or in the lumen of another organ (1).

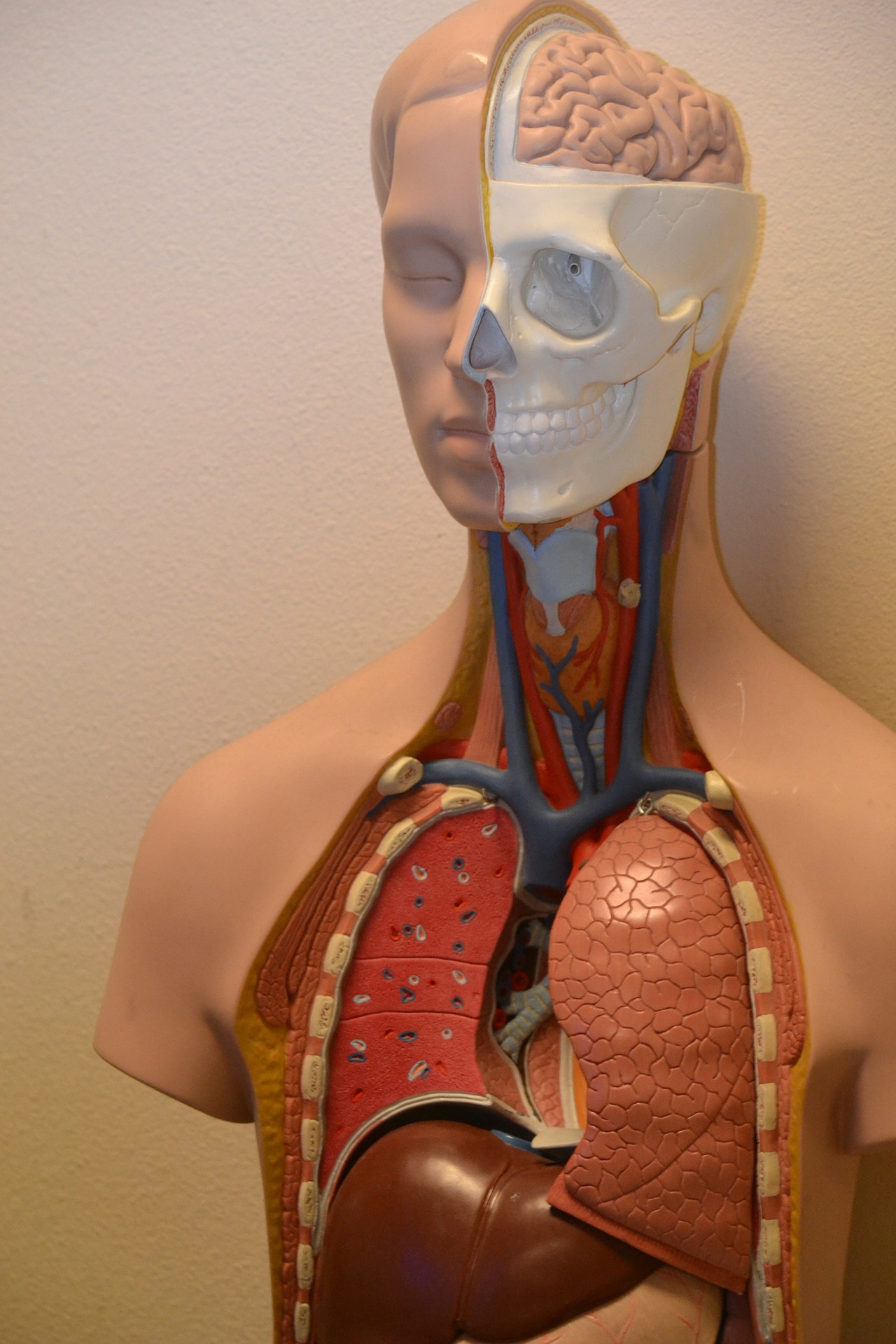
AnPhys3e-Fig-15-01-0R.png
Organs that Secrete Hormones
- Hypothalamus: The hypothalamus secretes several neurohormones that stimulate or inhibit anterior pituitary gland function (1).
- Heart: The heart makes atrial natriuretic peptide, which lowers blood Na+ (1).
- Adrenal glands: The adrenal glands make epinephrine and norepinephrine, mediating the fight-or-flight response (1).
- Cortex: The cortex makes aldosterone, which regulates Na+ and K+ balance; makes cortisol, which regulates growth, metabolism, development, immune function, and the stress response; makes some androgens that play a role in reproduction (1).
- Liver: The liver produces insulin-like growth factor 1, which controls the growth of bones; secretes angiotensinogen, a precursor required for the production of angiotensin II (1).
- Kidneys: The kidneys secrete erythropoietin, which regulates the maturation of red blood cells; produce the active hormone 1, 25-dihydroxy vitamin D; secrete the enzyme renin, which begins synthesis of the hormone angiotensin II (1).
- Pancreas: The pancreas makes insulin, decreasing blood glucose and glucagon, which increases blood glucose (1).
- Blood vessels: Cells of many blood vessel walls express enzymes required to complete angiotensin II synthesis, maintaining normal blood pressure (1).
- Adipose tissue: The adipose tissue produces hormones (for example, leptin), which regulate appetite and metabolic rate (1).
- Anterior pituitary gland: The anterior pituitary gland produces hormones with various metabolism, reproduction, and growth actions (1).
- Posterior pituitary: The posterior pituitary secretes oxytocin, which stimulates uterine contractions during birth and milk secretion after birth; secretes an antidiuretic hormone that increases water reabsorption in the kidneys (1).
- Pineal: The pineal gland makes melatonin, which may play a role in circadian rhythmicity (1).
- Parathyroid: The parathyroid gland makes parathyroid hormone which increases blood Ca2+ and stimulates the kidneys’ active form of vitamin D (1).
- Thyroid: The thyroid makes thyroid hormone, which regulates metabolic rate, growth, and produces calcitonin, which plays a role in Ca2+ homeostasis in some species (1).
- Stomach and small intestine: The stomach and small intestine secrete numerous hormones such as gastrin, secretin, and cholecystokinin that regulates pancreatic activity, facilitate digestion, and control appetite (1).
- Ovaries: Ovaries produce estrogens-such as estradiol and progesterone, which controls female reproduction (1).
- Testes: The testes produce androgens, such as testosterone, which control reproduction (1).

AnPhys3e-Fig-15-01-0R.png
Hormone Structures and Synthesis
Amine Hormones
- The amine hormones are derivatives of the amino acid tyrosine. Thyroid hormones include amine hormones (1). Catecholamines, epinephrine, norepinephrine, and dopamine are also types of hormones.
There are two adrenal glands, the adrenal medulla, and adrenal cortex. These both secrete steroid hormones. The adrenal medulla releases secretions into the blood. The adrenal medulla secretes epinephrine and norepinephrine. There is usually more epinephrine secreted than norepinephrine (1).

AnPhys3e-Fig-15-01-0R.png
Dopamine is the other catecholamine hormone that the hypothalamus synthesizes. Dopamine release into a portal system, which carries to the pituitary gland (1).
Peptide and Protein Hormones
Most hormones act as polypeptides. Peptide hormones synthesize on endocrine cells’ ribosomes then cleave to prohormones, which are enzymes in the rough endoplasmic reticulum (1).
The prohormone is packaged into secretory vesicles by the Golgi apparatus. The prohormone yields the active hormone and releases it into the vesicles by exocytosis. An example of this is insulin. Insulin is a preprohormone with C-peptides that secretes regular amounts in certain conditions in the body (1).
Synthesis (prohormone)- Packaging (hormone)- Storage (Hormone)- Secretion (Hormone).
Steroid Hormones
Steroid hormones are the third family of hormones. They are known as gonads, testes, ovaries, as well as the placenta (1).
Steroid hormones link to Gs proteins, and they activate adenylyl cyclase and cAMP production (1).
Protein kinase A by cAMP results in the phosphorylation of numerous intracellular proteins.
Steroid hormones derive from cholesterol, then get taken up by extracellular fluid by cells and intracellular enzymes (1).
The final steroid hormone expresses upon the cell type, and the amount of the enzyme increases.
Steroid hormones lack storage in the cytosol because of their lipophilic nature. Instead, they synthesize themselves. This process includes steroid hormones diffusing across the plasma membrane into the circulation (1).
Lipid steroid hormones are not highly soluble in blood. The majority of steroid hormones are reversibly bound in plasma to carrier proteins such as albumin and other specific proteins (1).

AnPhys3e-Fig-15-01-0R.png
Hormones of the Adrenal Cortex
Aldosterone is a mineralocorticoid and under the control of another hormone, angiotensin II. Angiotensin II binds to plasma membrane receptors in the adrenal cortex. After binding, there is an activation of the inositol triphosphate second-messenger pathway (1).
Cortisol and the steroid corticosterone are glucocorticoids. The term glucocorticoids come from the fact that they significantly affect glucose and other organic nutrients’ metabolism (1).
DHEA and androstenedione belong to the class of steroid hormones known as androgens. Androgens derive from the testes, and testosterone is the primary male hormone derived from the testes (1).
The adrenal cortex has the outer layer, the zona glomerulosa. This layer expresses the enzymes required to synthesize corticosterone and then convert it to aldosterone. However, the conversion does not represent the gene that codes for the enzymes needed to form cortisol and androgens (1).
Congenital adrenal hyperplasia, or CAH, is an excess amount of adrenal androgen production that results in virilization of the genitalia of female fetuses at birth (1).

Hormones of the Gonads
Hormones of the gonads include estrogens, which are known as estradiol and estrone. As well as estriol, which is the predominant estrogen present during a woman’s lifetime (1).
The cholesterol conversion includes the conversion of cholesterol to pregnenolone. After, pregnenolone converts to dehydroepiandrosterone. Finally, the last transformation is to androstenedione (1).
Cholesterol also converts to pregnenolone and converts to 17-Hydroxyprogesterone and finally cortisol or androstenedione (1).
Progesterone also converts to corticosterone, which then converts to aldosterone (1).
Progesterone also changes to 17-Hydroxygrogestorne, which then transforms to cortisol and androstenedione. Cholesterol changes to androstenedione to aromatase and then estrone (1).
Androstenedione also converts to testosterone, which secretes by testes and converts to estradiol by aromatase. The ovaries secrete aromatase. Estradiol also changes to estrone (1).

Hormone Metabolism and Excretion
A hormone’s concentration in the plasma depends on its secretion rate by the endocrine gland and its removal rate from the blood (1).
The liver and kidneys are the major organs that metabolize or excrete hormones (1).

AnPhys3e-Fig-15-01-0R.png
Metabolism of a hormone activates the hormone rather than inactivates it. The secreted hormone may be inactive until metabolism transforms it (1).
The thyroid gland produces T4, which converts to T3 inside the target cell (1).
Mechanisms of Hormone Action
- Peptides and catecholamines have a significant form in plasma and are free and unbound. The location is in the plasma membrane, and some signaling mechanisms are second messengers, enzyme activation by receptors, and intrinsic enzymatic activity of the receptor. The rate of secretion is fast in these mechanisms (1).
- Steroids and thyroid hormones are protein-bound and are intracellular. The most common signaling mechanisms are intracellular receptors that directly alter gene transcription. These are known for the slow rate of metabolism (1).
Up-regulation is an increase in the number of a hormone’s receptors in a cell (1).
Down-regulation is a decrease in receptor number, often from exposure to high hormone concentrations (1).
Permissiveness means that hormone A must be present for hormone B to exert its full effect (1).
Events Elicited by Hormone-Receptor Binding
Steroid and thyroid hormones are lipophilic. The receptors are intracellular and members of the nuclear receptor superfamily (1).
Pharmacological effects can also occur in diseases involving the secretion of excessive amounts of hormones (1).
Inputs that Control Hormone Secretion
Hormone secretion is mainly under the control of three types of inputs to endocrine cells. These can be changes in the plasma concentrations of mineral ions or organic nutrients. Neurotransmitters released from neurons end on the endocrine cell, while another hormone acts on the endocrine cell (1).

AnPhys3e-Fig-15-01-0R.png
Control by Plasma Concentrations of Mineral Ions or Organic Nutrients
As plasma glucose concentration increases due to eating food, the plasma insulin concentration increases. Actions of insulin increase; thus, there is the transport of glucose from extracellular to intracellular fluid. Calcium homeostasis is another form of calcium regulation (1).

AnPhys3e-Fig-15-01-0R.png
PTH or parathyroid hormone produces by cells of the parathyroid gland. A decrease in plasma Ca2+ concentration directly stimulates PTH secretion (1).
PTH exerts specifically on bone and other organ tissues. The exertion increases calcium release into the blood and restores plasma Ca2+ to standard levels (1).
Control by Neurons
Parasympathetic and sympathetic inputs affect hormones.
Control by Other Hormones

AnPhys3e-Fig-15-01-0R.png
Tropic hormone is a hormone that stimulates the secretion of another hormone.
The CNS central nervous system significantly affects hormones in the autonomic nervous system and impacts the adrenal medulla by converting it to the hormone epinephrine (1).
Hypothalamus can affect hormones and the anterior pituitary, which converts to hormones (1).
Types of Endocrine Disorders
Hyposecretion means there is too little of the hormone.
Hypersecretion is an excessive amount of hormones.
Hyporesponsiveness is a decreased responsiveness for hormones.
Hyperresponsiveness is an increased responsiveness of the target cells (1).
Type 2 diabetes is the most common form of diabetes mellitus in which target cells of the hormone insulin are hyporesponsive to this hormone (1).

AnPhys3e-Fig-15-01-0R.png
Summary
- The endocrine system includes glands and organs that secrete hormones.
- Endocrine differs from exocrine in that exocrine secrete products in a duct.
- Amine hormones are iodine-containing thyroid hormones. The catecholamines secrete by the adrenal medulla and the hypothalamus.
- Steroid hormones are produced from cholesterol by the adrenal cortex. The gonads are from steroid precursors by the placenta during pregnancy.
- DHEA and androstenedione are two hormones from the adrenal cortex. Adrenal glucuronic, and the mineralocorticoid includes aldosterone and cortisol.
- Ovaries produce estradiol and progesterone, and testes produce testosterone.
- Peptide hormones and catecholamines circulate in the plasma.
- The liver and kidneys are significant organs that remove hormones from the plasma by metabolizing or excreting them.
- Intracellular receptors activated by steroid and thyroid hormones typically function as transcription factors; the result is increased synthesis of specific proteins.
- Control of Neural inputs is by parasympathetic and sympathetic innervation.
- Hyposecretion, hypersecretion, hyporesponsiveness, or hyperresponsiveness are all ways hormones release from the cells (1).

Control Systems Involving the Hypothalamus and Pituitary Gland
The pituitary gland or hypophysis lies in a pocket at the base of the brain. The pituitary gland connects to the hypothalamus by the infundibulum. The gland contains axons from neurons in the hypothalamus and small blood vessels (1).

AnPhys3e-Fig-15-01-0R.png
The anterior pituitary gland or adenohypophysis and the posterior pituitary lobe are called neurohypophysis (1).
Terminals release hormones into capillaries then drain into veins and general circulation (1).
The median eminence is the junction of the hypothalamus and infundibulum. The capillaries recombine to form the hypothalamus-hypophyseal portal vessels (1).
The portal system has one set of capillaries that drain into veins that form the second set of capillaries before emptying again on veins that return to the heart (1).
The vessels pass down the infundibulum and enter the anterior pituitary gland and drain into a set of capillaries known as the anterior pituitary gland capillaries (1).
Posterior Pituitary Hormones
The supraoptic and paraventricular nuclei’s cell bodies have axons that pass down the infundibulum. These axons then terminate in the posterior pituitary (1).
The hormone enters capillaries to be carried away by the blood returning to the heart (1).
The two posterior pituitary hormones are oxytocin and vasopressin (1).
Oxytocin involves two reflexes related to reproduction. Oxytocin stimulates the contraction of smooth muscle cells in the breast. This stimulation results in milk ejection during lactation. Oxytocin also stimulates the contraction of uterine smooth muscle cells until a baby is born (1). 
ADH or antidiuretic hormone increases the volume of water excreted in the urine. Thus ADH decreases water loss in the urine and conserves water production when a person is dehydrated (1).

Summary
The hypothalamus will increase hormone secretion, which will lead to a plasma hormone increase. This increase will then lead hormone 2 to rise in the anterior pituitary and increase plasma hormone 2. The third endocrine gland hormone secretes, leading to a rise in plasma hormone three and finally, affects target cells in hormone 3 (1).
Overall there are six hormones in the anterior pituitary (1).
FSH and LH (stimulating follicle hormone and luteinizing hormone ) affect the gonads, which secrete hormones in men and females. Estradiol and progesterone secrete in females and testosterone in males (1).
Growth hormones secrete IGF-21 in the liver and help protein synthesis, carbohydrate, and lipid metabolism for organs and tissues. IGF is an insulin-like growth factor and directly affects bone growth and metabolism (1).
TSH (thyroid-stimulating hormone) secretes thyroxine and triiodothyronine (1).
Prolactin secretes in the breasts and is essential for breast development and milk production (1).
ACTH (Adrenocorticotropic hormone) will secrete in the adrenal cortex and will secrete cortisol (1).

Hypophysiotropic hormone
Hormones will diffuse out of anterior pituitary gland capillaries into the interstitial fluid. Upon binding to specific membrane-bound receptors, the hypothalamic neurons stimulate or inhibit the different anterior pituitary gland hormones’ secretion (1).
In essence, hypothalamic neurons affect hypophysiotropic hormones—the hormones will target capillaries in the median eminence (1).
The hypothalamo hypophyseal portal vessels in the anterior pituitary gland capillaries will flow into other cells (1).
Posterior pituitary hormones enter capillaries that drain directly into circulation (1).
CRH (corticotropin-releasing hormone) secretes into growth hormone (growth hormone-releasing hormone) and then releases TRH. This release will secrete GnRH gonadotropin-releasing hormone (1).

In summary
GnRH in the hypothalamus will release FSH and LH in the anterior pituitary (1).
GnRH will stimulate growth hormone in the anterior pituitary (1).
SST will inhibit growth hormone in the anterior pituitary (1).
TRH will activate TSH in the anterior pituitary (1).
Dopamine in the hypothalamus will inhibit prolactin in the anterior pituitary (1).
CRH in the hypothalamus will activate ACTH in the anterior pituitary (1).
There is long-loop negative feedback in cases like this, which means that hormone three will affect hormone 1 or 2 and inhibit those hormones from preventing hormone three from releasing too much (1).
Long loops also turn into short cycles.

AnPhys3e-Fig-15-01-0R.png
Summary
- The pituitary gland contains the anterior pituitary gland and the posterior pituitary. These glands are connected to the hypothalamus by the infundibulum (1).
- Axons in the hypothalamus release oxytocin and vasopressin in the posterior pituitary (1).
- The anterior pituitary contains GH, TSH, ACTH, prolactin, FSH, and LH (1).
- Hypophysiotropic hormones control the anterior pituitary (1).
- Long and short loop feedback inhibits or increases hormones (1).
Synthesis of Thyroid Hormone
Thyroid hormones are thyroxine or T4 and triiodothyronine T3. T4 converts to T3.
Pendrin is a protein that is an integral membrane protein that helps transport iodide ions to the follicular epithelial cells’ apical membrane (1).
The colloid of the protein contains a protein called thyroglobulin (1).
Once in the colloid, iodide will oxidize at the epithelial cell’s luminal surface to iodide (1).
Thyroglobulin is also synthesized by the follicular epithelial cells and secreted by exocytosis (1).
Thyroid peroxidase is an enzyme responsible for oxidizing iodides and attaching them to thyroglobulin (1).
Monoiodotyrosine is a tyrosine with one iodine attached to it. The molecule of the monoiodotyrosine is removed and coupled to another thyroglobulin molecule. When two tyrosine molecules combine, such as a diiodotyrosine, the result is thyroxine or T4 (1).
Therefore, one monoiodotyrosine and one diiodotyrosine result in T3 (1).
For thyroid hormone to secrete into blood, endocytosis is the engulfing portions of the colloid and brings it to contact with lysosomes. Then proteolysis of the thyroglobulin will release T4 and T3 and diffuse into the cell (1).

Summary
- TRH secretes in the hypothalamus.
- TRH plasma increases in the hypothalamus-hypophyseal portal vessels.
- Anterior pituitary will have the TSH secrete.
- TSH will increase plasma.
- T3, T4, secretes thyroid hormone.
- Plasma thyroid hormone increases.
- T4 converts to T3, and these are target cells for thyroid hormone.
Summary (another way to describe the events)
- Iodide is a cotransporter with Na+.
- There is diffusion into the lumen of the follicle.
- Iodide is transported, oxidized, and attached to rings of tyrosine.
- Iodinated ring of one monoiodotyrosine or diiodotyrosine adds to a DIT at another spot.
- Endocytosis of thyroglobulin of T3 and T4 takes place.
- Lysosomal enzymes release T3 and T4 and secretes these ions.
Control of Thyroid Function
Hypertrophy of thyroid cells is possible if exposed to more significant amounts of TSH. The thyroid gland enlarges due to this process and is called a goiter (1).
Actions of Thyroid Hormone
T3 has many actions through organs and tissues and induces gene transcription and protein synthesis (1).
T3 has effects on carbohydrate and lipid metabolism. This energy is through Na+/K+ ATPases through the body due to enzymes stimulated by T3 (1).
Homeostasis maintains by control of ATP and stored and used for an increase in glycolysis. This process is critical to the body’s metabolism as control of T3 stimulation can regulate body temperature and overall physiology when there are adequate stores of ATP and negative feedback loops are in place to handle T3 (1).

Permissive Actions
When there is an excess of T3, drugs that block beta-adrenergic receptors help alleviate anxiety, nervousness, and racing heartbeats (1).
Growth and Development
Congenital hypothyroidism is a condition in which there is an absence of T3, which results in a poorly developed nervous system and severely compromised intellectual function (1).
The cause is due to dietary iodine deficiency in the mother when the fetus is growing. Treatment usually starts in the neonatal period. If not, then congenital hypothyroidism is irreversible (1).
Hypothyroidism
Hypothyroidism is when the thyroid has low concentrations and is deficient in iodine. This intense concentration leads to an increase in TRH and TSH and, ultimately, an overiodization of the thyroid gland, which will cause goiter (1).
Autoimmune thyroiditis is a condition in which there is an autoimmune response of the thyroid gland. One form of this is called Hashimoto’s disease, in which cells of the immune system attack thyroid tissue (1).
Treatment of iodine replacement through a pill can cause normal function of the thyroid (1).
When T3 is too low, hydrophilic molecules accumulate and can cause myxedema (1).
Hyperthyroidism can develop from tumors of the thyroid gland and create an autoimmune disease called graves’ disease. Grave’s idea is a condition in which TSH receptors are overstimulated and increase the thyroid gland’s activity (1).
Hypothyroidism can cause cold intolerance. In comparison, hyperthyroidism can cause heat intolerance, weight loss, and increased appetite (1).
Introduction-The Physiology of Stress

The physiological link of stress ties into what is known as cortisol. Our brain consists of several regions, some of which include the forebrain, midbrain, and hindbrain. The forebrain contains areas like the frontal cortex, which consists of the diencephalon and the cerebrum. Within the diencephalon are two main areas, which are called the thalamus and hypothalamus. The thalamus is responsible for coding sensory input, while the hypothalamus is a significant region of the brain in which hormones facilitate themselves through different body sites (1).
The hypothalamus has two areas; the anterior pituitary and the posterior pituitary. The anterior pituitary releases hormones adrenocorticotropic hormone (ACTH) and thyroid-stimulating hormone.
Other hormones include (TSH), growth hormone (GH), prolactin, gonadotropin-releasing hormone, or GnRH. These hormones release signals into the blood that circulate to distant areas of the body and cause some response (1).
Corticotropin-releasing hormone or CRH is an amino acid peptide released by the hypothalamus. The release is due to stressful stimuli. This peptide secretes ACTH from the anterior pituitary. The ACTH secretes from the anterior pituitary and releases into capillary beds within the pituitary. The hormone eventually gets taken into the blood and released throughout the body. These hormones find their way into the adrenal cortex (1).
Finally, cortisol releases within the adrenal cortex from cell bodies known as the zona fasciculata. The cell bodies are named glucocorticoids and are responsible for the body’s metabolism. Cortisol is so essential that during times of stress, the body needs to regulate blood glucose. Cortisol assists in increasing levels of glucose metabolism during stress through a method called catabolism (1).
Catabolism is a method used by the body to break down essential fatty acids and glucose for fuel. This increase in regulation and breakdown gives us the energy that we need to carry out a task. The body finds itself in a very original state during catabolism due to other physiological factors, such as increased heart rate from the sympathetic nervous system, leading to higher cardiac output.
The increase in cardiac output means that more oxygen and nutrients utilize in the body’s tissues, such as skeletal muscle.
This form of physiology prepares an individual for the classic “flight or fight” response. The hormones epinephrine and norepinephrine allow humans to react quickly to any particular stimulus (1).
The exciting thing about cortisol is that it can have very beneficial effects in the short term, although the long-term immune function can severely suffer. This fact is primarily correct for individuals who are already compromised in their immune system or have chronic diseases such as asthma, diabetes, or cardiovascular disease (1).
Adrenal Insufficiency and Cushing’s Syndrome
Adrenal insufficiency is due to the loss of adrenocortical function.
Infectious diseases occur as tuberculosis and infiltrate the adrenal glands by destroying them (1).
Hypotension is low blood pressure, and Addison’s disease is a primary adrenal insufficiency (1).
Cortisol concentration is below normal during adrenal insufficiency. Inadequate ACTH secretion can also cause secondary adrenal insufficiency, which arises most of the time from the pituitary gland (1).
Cushing’s syndrome is a state where there is excess cortisol in the blood. Cushing’s syndrome can, at times, cause diabetes due to the excess of cortisol. Alternatively, even hypertension, which is a case of high blood pressure. Cushing’s disease is when ACTH secretes a tumor of the anterior pituitary gland (1).
Low cortisol in the body results in osteoporosis. Osteoporosis is a disorder that causes brittle bones and results in weak bone strength (1).
Other Hormones Released During Stress
Aldosterone, vasopressin, growth hormone, glucagon, and beta-endorphin also release due to stress (1).
Insulin secretion decreases while vasopressin and aldosterone retain water and Na+ within the body during stress (1).

AnPhys3e-Fig-15-01-0R.png
Bone Growth
A bone divides into epiphyses, and the remaining middle part is called the shaft (1).
Each epiphysis comes in contact with the shaft. As well as proliferating cartilage comes in connection with the epiphyseal growth plate (1).
Osteoblasts are the forming cells, while cells called chondrocytes simultaneously lay down new cartilage in the plate’s interior (1).
The linear growth of the shaft can continue as long as the epiphyseal growth plates exist. Scientists determine bone age by taking an X-ray of bones and deciding which ones have undergone epiphyseal closure, which is the point in time where growth plates convert to the bone as a result of hormonal influences (1).

Hormonal Influences on Growth
T3, insulin-like growth factors 1 and 2, insulin, testosterone, and estradiol are all-important hormones for growth (1).
IGF-1 is essential for maintaining growth, and when deficient, it can result in a person having a short stature or decreased growth (1).
IGF–1 secretes by the liver, enters the blood, and functions to stimulate chondrocyte precursor cells in the bones. They can act as autocrine or paracrine substances to promote cell division. The influxes of IGF-1 are maintenance by growth hormones (1).
Summary Growth Hormone
- Growth hormone promotes the growth of IGF-1 cells in cell division.
- Growth hormone stimulates protein synthesis in muscle.
- Anti-insulin effects mean that adipocytes are more responsive to stimuli in breaking down triglycerides. Anti-insulin stimulates gluconeogenesis and reduces insulin’s ability to stimulate glucose uptake by adipose and muscle cells.
Summary IGF-1
- A stimulus such as IGF-1 is essential for regulating stress, fasting, or sleep.
- The hypothalamus increases GnRH secretion.
- GnRH goes into the plasma GnRH or hypothalamus-hypophyseal portal vessels.
- Anterior pituitary increases GH secretion.
- The secretion goes into plasma GH.
- Finally, the liver secretes IGF-1 secretion.
IGF-2 is another growth factor related to the prenatal period (1).
T3 hormone increases for growth due to stimulation of chondrocytes defecation. The development also causes new blood vessels (1).
Insulin is a hormone that is essential for the transport of glucose and the storage of fat. It also affects cell differentiation directly (1).

Sex steroids are essential for puberty, so when testosterone and estradiol in males and females increase, sex steroids will lengthen bones and rapidly regulate behavior and emotions (1).
Effector Sites for Ca2+ Homeostasis
Bone is a connective tissue made up of several cell types surrounded by a collagen matrix called osteoid (1).
These minerals release calcium, phosphate, and hydroxyl ions are known as hydroxyapatite (1).
Mineralization is the process in which collagen forms around a matrix (1).
Osteoblasts transform into osteocytes once the matrix is calcified (1).
Osteoclasts are large cells that break down formed bone by dissolving the ions and secreting hydrogen ions (1).
Bone remodeling occurs by osteoblast, osteocytes, and osteoclasts working together (1).
Osteoclasts resorb old bone; osteoblasts move into the area, lay down a new matrix, and get mineralized (1).
Parathyroid hormone regulates by calcium concentration and is essential for bone health (1).

AnPhys3e-Fig-15-01-0R.png
Kidneys
Kidneys filter blood and excrete wastes.
Calcium’s urinary excretion is the defense between the amount filtered into the tubules and the amount reabsorbed (1).
Reabsorption of calcium decreases as plasma calcium concentration increases. As calcium increases, plasma calcium decreases (1).
Phosphate ions, as well as calcium, are reabsorbed or secreted through this process (1).
Gastrointestinal Tract
Solutes such as Na+ and K+ from the gastro tract usually are high. However, ingested calcium is not absorbed from the small intestine and leaves the body, along with feces (1).
That is why it is essential to have an active transport system that achieves calcium absorption and decreases excreted amounts (1).
Hormonal Controls
Parathyroid Hormone
PTH or parathyroid hormone is essential for calcium regulation.
PTH has extracellular calcium directly on the secretory cells via a plasma membrane calcium receptor (1).
Decreased plasma calcium contraction will stimulate PTH secretion, and plasma concentration does the opposite (1).
PTH Summary
- PTH increases the resorption of bone by osteoclasts.
- PTH stabilizes 1,25 dihydroxy vitamin D, which increases intestinal absorption of calcium and phosphate ions.
- PTH increases calcium reabsorption in the kidneys.
- PTH decreases the reabsorption of phosphate ions.
Calcium Summary
If there is low plasma calcium
- Parathyroid glands will secrete more in the plasma and ultimately increase calcium reabsorption in the kinesin. 1,25 OH2D formation and bone reabsorption also increase.
- This reabsorption leads to decreased calcium excretion and calcium absorption in the blood, and the overall restoration of plasma calcium returns to normal.
1,25 OH2 is formed from vitamin D2 and vitamin D3 and metabolizes into the enzyme 25-hydroxylase (1).
Vitamin D summary
Vitamin D2 or D3 turns into plasma vitamin D, or the same thing comes from the sunlight, which converts 7-dehydrocholesterol into vitamin D3 (1).
Vitamin D then converts into 25-OH D in the liver by 25-hydroxylase (1).
25-OH D converts to 1,25-OH2D by one hydroxylase and then increases calcium absorption in the GI Tract (1).
Metabolic Bone Diseases
Selective estrogen receptor modulators or SERMS act by interacting with estrogen receptors and increasing estrogen in menopause (1).
Low plasma calcium concentrations include hypercalcemia or hypocalcemia (1).
Hypercalcemia is a form of hyperparathyroidism where PTH in the adenoma is in excess (1).
There is an increase in calcium reabsorption from bone and the kidneys, as well as 1,25 OH2D. This change results in calcium absorption from the small intestine. This condition is a case of cancer treated by surgical removal of the parathyroid tumor (1).
Other forms of cancer lead to humoral hypercalcemia of malignancy. The cause of hypercalcemia is PTH-related peptide in which is produced by cancerous cells (1).
Treatment is due to treating the release of PTH.
Excessive ingestion of vitamin D also leads to hypercalcemia and causes significant symptoms, primarily in tissues and organs, resulting in muscle weakness, nausea, and vomiting (1).
Hypocalcemia is a state that results from losses of the parathyroid gland in the body. This function allows for 1,25 (OH)2D to decrease in this state (1).
Pseudohypoparathyroidism is a condition in which hypoparathyroidism symptoms are due to the PTH’s hyperresponsiveness (1).
This state occurs even when PTH concentrations in the blood elevate (1).
Secondary hyperparathyroidism is a failure to absorb vitamin D.
This state is also known as a hypokalemic state that only occurs in the intestines. This state decreases kidney 1,25-(OH)2D production and reduces intestinal absorption of calcium in the glands (1).
Hypocalcemia also leads to excitable tissue in the nerves. It also leads to seizures, muscle spasms (hypocalcemia tetany), and neuronal excitability (1).
Treatment involves giving calcium aids and 1,25-(OH)2D or vitamin D (1).

Summary
- 99% of total body calcium is in the bone as a mineral on a collagen matrix.
- Osteoblasts and osteoclasts remodel bone.
- The GI tract absorbs calcium.
- Amount filtered and reabsorbed means the difference in which calcium excretes.
- PTH increases calcium concentration as well as 1,25-(OH)2D.
- PTH inhibits phosphate ions.
- Osteoclasts and rickets disease are mineralized when the bone is deficient.
- Osteoporosis is a loss of bone density.
- Hypercalcemia or hyperparathyroidism is when there is too much PTH stimulation. This stimulation increases calcium reabsorption in the kidneys and intestines.
- Hypocalcemia or hypoparathyroidism leads to decreased bone resorptions of calcium and low production of 1,25-(OH)2D
- Secondary hyperparathyroidism is by vitamin D deficiency due to inadequate intake, absorption, and kidney activation (1).
This summary concludes the section on the endocrine system.
Sources
Hill, Richard W., et al. Animal Physiology. Oxford University Press, 2018.
Vander, Arthur J., et al. Vander’s Human Physiology: The Mechanisms of Body Function. McGraw-Hill Education, 2019.